“At 11 years old, I found myself running in my sixth-grade gym class, a mandatory activity. I couldn’t keep up like the athletes I was surrounded by, and I absolutely detested the activity. On this particular day, intense pain was spreading through my chest, head, and into my limbs. Eventually, my vision faded as I came to an abrupt halt and tried to walk the pain off. Not fully comprehending what just happened, my 11-year-old self dismissed the event, labeled it asthma, and I spent the rest of the year borrowing my friends’ inhalers.
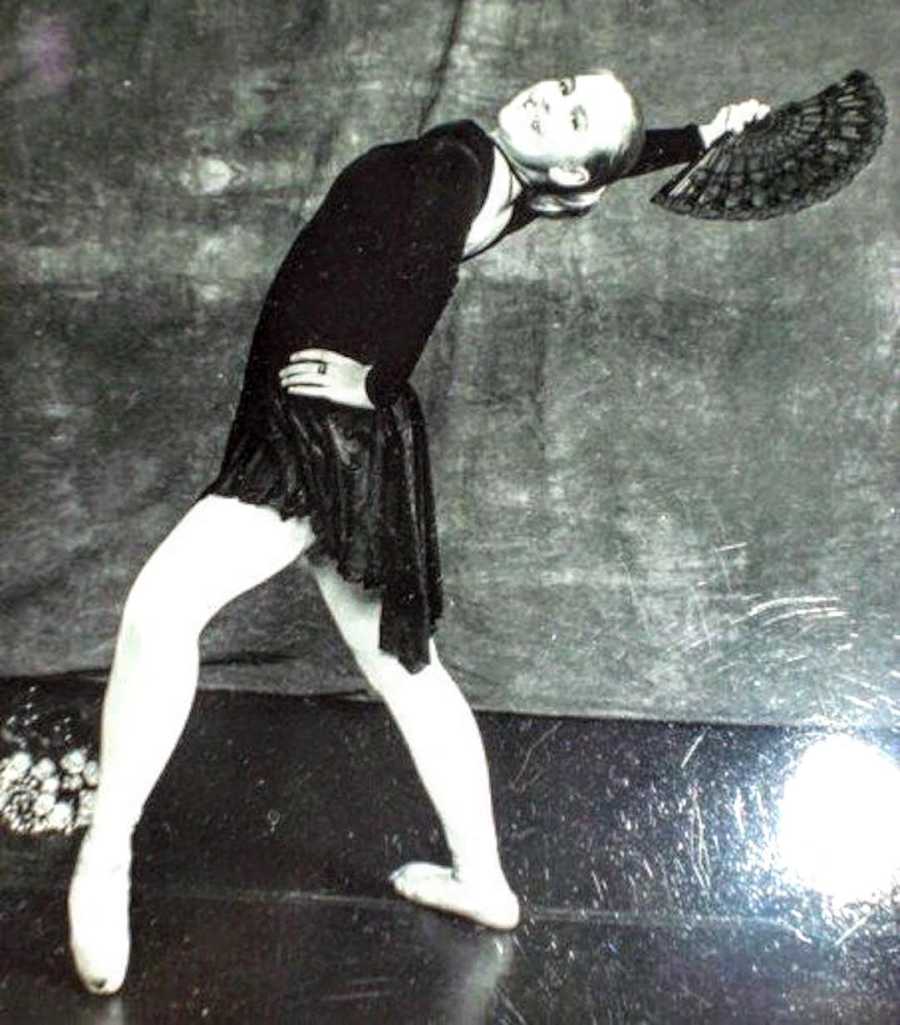
By the end of junior high, the painful ‘episodes’ began to show while walking upstairs, in my ballet classes, and even just walking into the mall. I spent my high school years completely unable to use the stairs, struggling to walk the hallways, and absolutely exhausted. Family doctors labeled me with exercise-induced asthma, weight problems. I left an emergency room visit with no answers and a negative pregnancy test because I was just a 16-year-old female who suspiciously passed out. I quit ballet and began to seriously limit my physical activity, as much as a high schooler can.
Growing into 17 with newfound independence of a car and a job, I began to give voice to the intense pain I experienced daily. ‘I don’t think I can walk at graduation,’ I spoke with my dad late one night. He listened quietly to how I felt, and all the internet research I had done on why I couldn’t breathe.
That week, we visited a local store to pick up graduation announcements. I struggled to keep up behind my father while walking in. Reaching the entryway, I managed to get the words, ‘I can’t breathe’ out, and lay completely down in the doorway with people shuffling around us. He held my wrist, counted my pulse, and finally saw for himself what I had been experiencing for the past almost 7 years.
My dad argued our way for an appointment into a cardiologist’s office (I was too young to be seen apparently) and we were scheduled for early July. My dad and brother accompanied me to the appointment and watched me struggle to walk into the office. Small distances were now a daily struggle, and I hoped finally the pain would be seen and given a name. The nurses took an EKG, which my father, being his critical-care paramedic self, read over their shoulders. Then they put an oxygen saturation monitor on my finger, which was simple confirmation no, I wasn’t too young to be here. ‘What’s the reading?’ I remember dad asking. ’85,’ she replied. My dad and brother gasped while I asked, ‘Is that bad?’ ‘It’s certainly not good.’ When the cardiologist entered the room he exclaimed, ‘Something is very wrong with you!’ I smiled, with the knowledge yes, finally, a professional believed me.

I left the office that day with a diagnosis of Atrial Septal Defect and a heart catheterization scheduled so they could measure the hole that apparently was in my heart. When the day arrived, it took the nurses eight tries to get a good enough IV started. I signed waivers giving certain permissions and assessing risks because I had been 18 a mere 3 weeks. Here was my stark welcome to adulthood. Wheeled into the OR, I was then told, ‘You have to be awake during the entire process.’ They relaxed me and followed with an esophageal tube to take pictures, followed by a threading sort of feeling from a wire being pushed through my femoral artery. I lay there for what felt like hours, watching black and white pictures of my vessels light up, and heart-pumping vigorously.
Finally, the lights flickered on and the cardiologist came to my side to say, ‘We couldn’t find the hole so the problem is not in your heart. It’s in your lungs. I need to talk to another doctor, then I will come to see you.’ How could they not find the hole? What is the problem? Do they even know? Do they still believe me? I cried through them trying to get my bleeding under control, and finally, I arrived in recovery where I was told my actual diagnosis. ‘What you have is Pulmonary Arterial Hypertension. There’s no cure, and if we do not find a successful treatment immediately, you are going to die.’

So much emotional energy swarmed that recovery room there was no space left over for me to feel anything. I wanted to be seen so badly and to have a diagnosis, only to be deeply unsatisfied with the results. In that cramped recovery room, denial, disassociation, and non-compliance were born. For almost 7 years, I half-comprehended what my doctors told me. I would decide life wasn’t worth living. I couldn’t have children. No one would want to be with me. I would be too expensive to keep alive, therefore I would abruptly stop treatment. I ingested the pills on and off when I pleased, and my father would beg me to be consistent with treatment exclaiming, ‘You’re going to die!’ I would laugh hysterically in response.
After a while, prayers disappear. People can only stomach a brave ‘strong fighter’ face. Feeling unstable and out of control, this image I was trying to uphold as ‘okay’ finally collapsed under the pressure of reality. It had been for quite some time. Yet, it was leaking out in substance abuse, rage, irrational behavior, and alienation. Everyone was growing up and having children of their own, and I was being pumped full of pills and attached to oxygen tanks. The denial and hatred continued until finally I was transferred, by pure luck, to a new specialist at the University of New Mexico.

Dr. Melendres sat me down with a blank piece of paper and drew out Pulmonary Arterial Hypertension, the different classes of it, and circled which one I was in. She explained how it’s progressive, aggressive, and we have to be aggressive right back. She walked her entire team through the room, and who would be in charge of what. Then walked in my social worker. Marty explained what she would help me with, what kinds of feelings I might be having, and what we needed to do about them. It took 8 years to find an aggressive new team that knew exactly who they were dealing with— a very non-compliant and grief-stricken patient.
Within 8 months, my Pulmonary Hypertension progressed rapidly. I found myself feeling worse than I did in the beginning, this time living in the mountains of New Mexico. I had a pericardial effusion, my cardiac output was extremely low, and I was at risk for sudden death. I had to look deep within to go ‘all-out’ and commit myself to a very aggressive therapy because, well, there were no more options. I was emergency-admitted to the University of New Mexico’s ICU and started intensive IV therapy.

After barely living through it, I was discharged and attached permanently to my IV infusion pump through my Hickman line that delivered the medicine directly into my heart. Learning to mix your own IV medication, work an infusion pump, and survive through chemo-like side effects was my first humble lesson in my new ‘artificially alive’ life. Then came obeying cleanliness orders of no swimming, submersion, tube changes, dressing changes, and overall a complete transition into a new reality. My friend and fellow patient, Sean, reminded me through my rage the pain of the reality of the pump would subside. I would just be alive, and it would be enough.

As I transitioned into understanding compliance, I watched my friends and fellow patients die one by one throughout 2018 – Sean included. Almost my entire friend group filled with young, beautiful, and talented people were all taken one after another. It became the feeling of walking into a battlefield with your platoon, only to look around and somehow you were one of the only ones left standing. Was I next? Was another one of my friends next? After a severe mental breakdown that endangered my health, I sought out a therapist who could undo the severe paranoia, apparent survivor’s guilt, and self-hatred. 8 years after my diagnosis, I was diagnosed with Complex-Post Traumatic Stress Disorder. Finally, a crucial piece of the puzzle had been revealed to me your mental health is indeed your health, not an accessory to your healthcare.
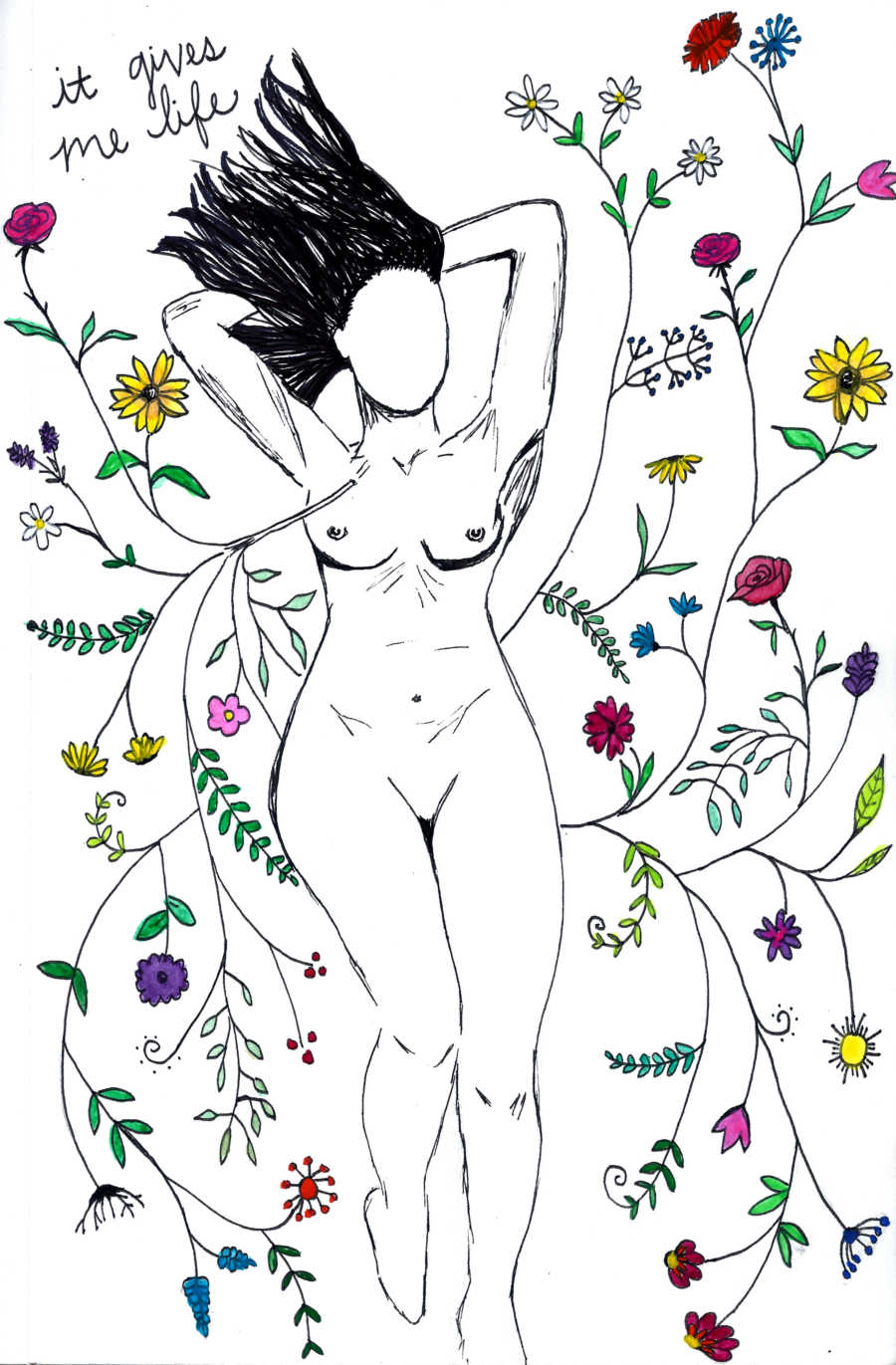
2 years after consistent therapy, art has been a significant help in my existence. Working through difficult emotions almost too complex to put words to, and of course finding relief in finally being a compliant patient working with my doctors to save my own life, no matter how much I despise my organs sometimes. I write today still on the road to acceptance of myself. Acceptance of my weight, death, my mental health, my flaws, my tubing, the machine on the other end of it, and my lungs. Society convinced me for a long time that I didn’t have the correct ingredients for happiness and success. Sometimes, I will still catch my mind observing and critiquing myself in comparison to others, with the conclusion I have failed somehow.
Through people’s empathy and honesty about who they really are and how different life can be for all of us, I have learned there is no correct list for the makeup of happiness or success. Most importantly, there is no normal. It took nearly 8 years to truly understand I was terminal, traumatized, and terrified because America was telling me everything was just fine if I would stay positive. Except, I had a tube in my chest, was mixing my own IV meds, throwing up daily, insurance was denying everything, the government didn’t want to cover pre-existing conditions anymore, and my friends were dropping dead. I was running through a blood-filled battlefield with corpses everywhere only I could catch sight of. Your perception of reality is a fight for survival that is vastly too intense for others, especially when the reaction is what your brain is currently wired to produce.
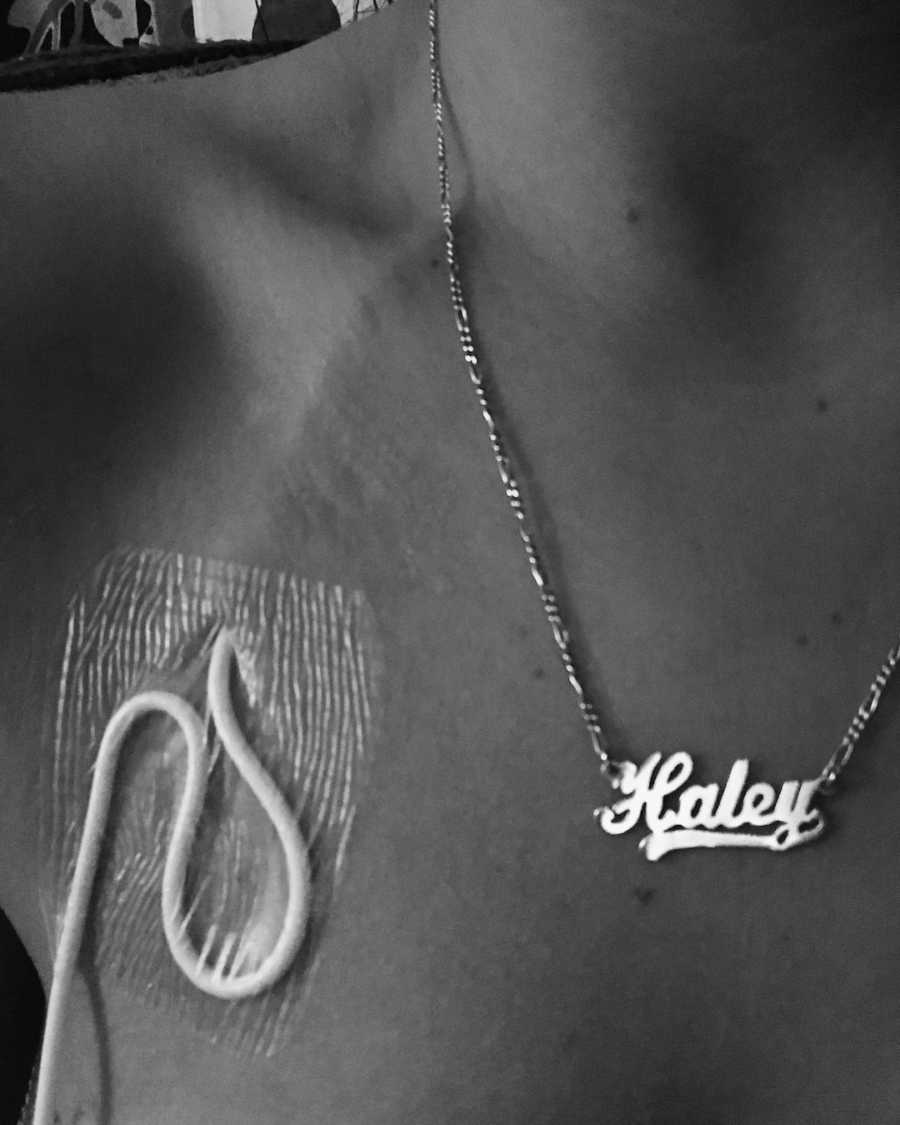
Just having the courage to acknowledge this disease and disability is indeed trauma was a step further into how much power I gave that battlefield in my life. It became a balancing act of recognizing when my brain wants to tell me I’m in danger because it sensed a trigger, versus when I’m actually in danger. And how to calmly navigate through these perceived and sometimes very real threats. Accepting that my brain and I had changed has been crucial in my recovery. I will never be the same because the skin that holds my body together has new tubes, scars, and sheds repeatedly. The truth is unpalatable, alienating, and disturbing. Underneath its crushing embrace, I collapsed into this final form of who I had no choice in becoming. I just am.”

This story was submitted to Love What Matters by Haley. You can follow her story on Instagram. Submit your own story here, and subscribe to our best stories in our free newsletter here.
Read more stories like this:
Provide strength and encouragement for others. SHARE this story on Facebook with friends and family.

